With the widespread use of ultrasounds, a diagnosis of prenatal hydronephrosis is becoming increasingly common. Learn more about what it is, it’s causes and treatments
What is prenatal hydronephrosis?
What are the causes of prenatal hydronephrosis?
- Physiological: This is seen during the early development of the urinary tract. The majority of such cases are transient and resolve on their own
- Blockage: The most common pathology underlying this disease is some kind of blockage seen at the pelvic ureteric junction (PUJ), the region where the ureter meets the kidney. A blockage can also occur at the vesicoureteric junction (VUJ), the region where the ureter meets the bladder, or in the posterior urethral valve
- Urine reflux: Vesicoureteral reflux is the backflow of urine from the bladder into the kidneys. This usually occurs when the valve between the bladder and the ureter is incompetent
- Anatomical defects: In rare cases, for example, if the baby has two collecting tubes instead of one, it can either directly lead to backflow or urine or give rise to further obstruction (hydrocoele). Such defects can usually be picked up on ultrasound
- Prune Belly syndrome: This is characterised by a triad of incomplete development of the abdominal muscles, urinary tract abnormalities and undescended testicles
What are the signs and symptoms of prenatal hydronephrosis?
How can prenatal hydronephrosis affect my baby?
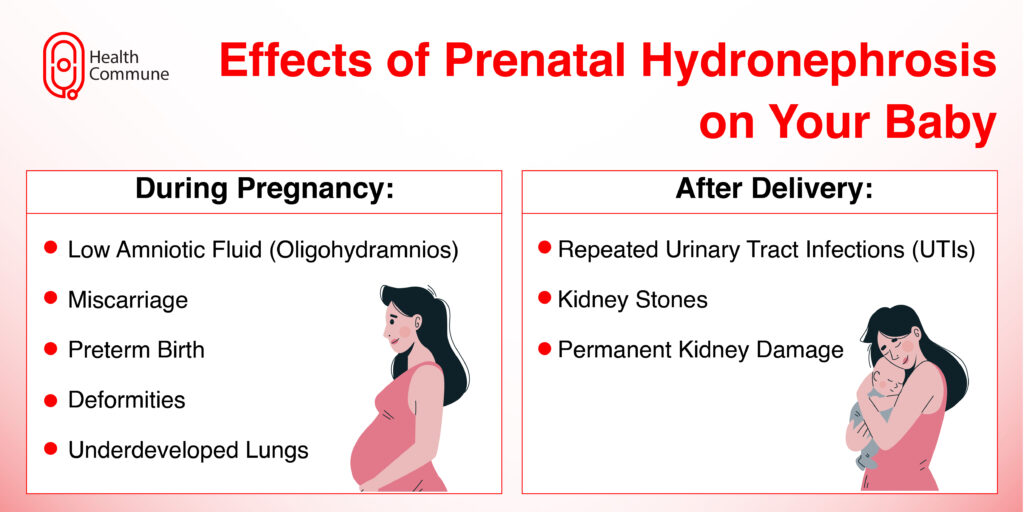
In severe cases during pregnancy, the volume of amniotic fluid may become very low, a condition called oligohydramnios (since your baby’s urine is the main component of this fluid). This can lead to serious complications for your baby, such as miscarriage, preterm birth, deformities, and underdeveloped lungs.
After delivery, it can lead to the following complications:
- Repeated urinary tract infections
- Kidney stones
- Permanent kidney damage
How is prenatal hydronephrosis diagnosed?
It is diagnosed through an ultrasound scan. Your doctor will recommend routine prenatal scans to monitor your baby and look out for complications. Based on the findings prenatal hydronephrosis is divided into mild, moderate and severe.
If your baby’s scan is normal after birth your doctor will perform a follow-up scan at 1 to 1.5 months. If your baby has moderate swelling of the kidneys, a follow-up scan will be additionally done at 3 and 6 months and then every half or one year until the condition dissolves.
In severe cases, your doctors can recommend additional scans such as:
- Micturating cystourethrogram (MCU): In case there is significant dilatation in your newborn’s ureters, your doctor will perform an MCU at around 1 to 1.5 months to determine the presence of vesicoureteric reflux
- Diuretic renal dynamic (DTPA) scan: If your doctor has ruled out vesicoureteric reflux, they can perform a DTPA scan to detect obstruction at the pelvic ureteric junction (PUJ) or the vesicoureteric junction (VUJ)
Can prenatal hydronephrosis go away on its own?
What can I do to prevent my baby from developing hydronephrosis?
What is the treatment for prenatal hydronephrosis?
When does my baby need surgery?
If your baby has severe or worsening hydronephrosis, high-grade obstruction or repeated urinary tract infections (UTIs), your doctor will recommend surgery to improve urine flow and prevent any complications.
Your doctor can perform a pyeloplasty, which are cutting out a part of the blocked ureter in the case of a PUJ obstruction. If your baby has a posterior urethral valve, your doctor can perform a primary valve ablation.





