Piles got you at the edge of your seats? Find out more about the causes, types, stages, symptoms, and treatment options here.
What are piles (haemorrhoids)?
Piles, or haemorrhoids, are swollen blood vessels in the lower part of the rectum or anus. They can lead to bleeding and discomfort.
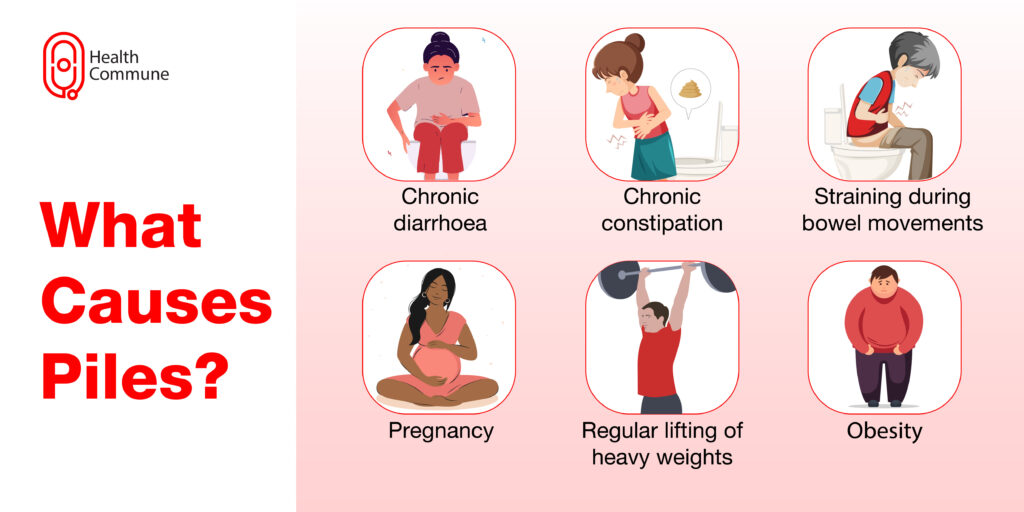
What causes piles?
While their exact cause is unknown, certain associated conditions include:
- Chronic constipation
- Chronic diarrhoea
- Straining while passing stools
- Regularly lifting heavy weights
- Pregnancy
- Obesity
What are the types of piles?
Depending on their location, they can be internal or external. The former develops in the rectum, while the latter develops under the skin around the anus.
What are strangulated piles?
If the blood supply to internal piles gets cut off, it can get ‘strangulated’ and cause severe pain. Consult your doctor immediately if you think you’re suffering from this condition.
What are the different stages of piles?
Piles can be divided into four stages, ranging from mild to severe, depending on the level of prolapse. Your doctor will recommend the appropriate treatment for you based on this.
- Grade 1 has small swellings on the inside of the anus. They cannot be seen or felt from outside the anal canal.
- Grade 2 has slightly larger swellings. They may protrude while passing stools but go back inside on their own once the pressure decreases
- Grade 3 are swellings that protrude outside the anal canal but can be pushed back with your fingers
- Grade 4 is the most severe; the swellings are permanently outside the anal canal and cannot be pushed back manually
What are the symptoms of piles?
You may notice the following symptoms:
- Painless, bright red-coloured blood while passing stools
- Discomfort while passing stools
- Itching around the anus
- Swellings in the anal region
- Leaking of stools
How are piles diagnosed?
Your doctor can diagnose this condition based on your symptoms and a simple physical examination. External piles are usually visible, while internal piles can require an examination of your anal canal and rectum as well.
- Digital examination: Your doctor will insert a gloved, lubricated finger inside your anus and check for any swellings, growth or tenderness
- Proctoscopy: A short, straight tube called a proctoscope is used to examine your anus and rectum to detect any abnormalities
- Colonoscopy: Your doctor may opt for a detailed bowel examination to help rule out other conditions
How are piles managed?
Your doctor may prescribe:
- Topical lignocaine or hydrocortisone cream which can be directly applied to the affected area and provide relief
- Suppositories which can be inserted inside the anus help relieve pain and discomfort
- Stool softeners to help pass motion more easily without straining
- Banding treatment is where a band is placed around the affected blood vessel to make it drop off
- Injection sclerotherapy is where a chemical is injected into the blood vessel to shrink it so that it drops off after a few days
- Electrotherapy and diathermy which use heat to shrink the blood vessel
- Infrared coagulation, where infrared light is used to cut off the blood supply to the vessel
- Surgery, in severe cases
What are the surgeries for piles?
Surgery is a safe and efficient treatment option. Commonly done procedures include:
- Haemorrhoidectomy, where your piles are surgically removed
- Stapled haemorrhoidopexy where the blood supply is cut off
- Haemorrhoidal artery ligation where the small arteries that are supply blood are tied
What happens in haemorrhoidectomy?
In haemorrhoidectomy, the piles are tied up and removed. You’ll be made to lie in the ‘lithotomy position’ (you will lie back with your legs spread apart, raised and supported by stirrups) while your surgeon gives you anaesthesia (local or general anaesthesia), dilates your anal canal and makes an incision to remove the affected tissue. It can be done either by open technique, where the skin around the affected region is left open so that it naturally heals or by closed technique, where the wound is closed by suturing.
In how many days can I get back to my routine activity post-surgery?
You can resume your normal activities within 2-3 days after the surgery.
What are the potential complications of surgery?
Complications rarely occur post-surgery. These can include:
- Bleeding or passing blood clots
- Infections
- Urinary retention
- Faecal incontinence
- Anal fistula
Is there a chance of relapse after surgery?
Relapse after surgery is uncommon but may happen if you follow an unhealthy lifestyle.
Are there any home remedies for piles?
Mild cases can be relieved by:
- Consuming a fibre-rich diet with lots of fresh fruits and vegetables and wholewheat grains such as brown rice, oats, ragi, and millets to avoid straining while passing stools
- Soaking your anal region in a warm bath or sitz bath 2-3 times a day to provide relief
- Using oral painkillers such as paracetamol or applying topical creams over the affected area
How can I prevent piles?
You can incorporate certain dietary and lifestyle changes such as:
- Staying well hydrated
- Consuming a fibre-rich diet with lots of fresh fruits and
- vegetables, wholewheat grains such as brown rice, oats, ragi,and millets
- Avoid straining while passing motion
- Taking a warm bath to reduce itching and discomfort
- Using ice packs over the region to reduce pain
- Keep your anal region as clean and dry as possible Regularly exercise at least 2.5 hours a week
What is the difference between piles, anal fissures, and fistulas?
An anal fissure is a small tear in the lining around the anus. It can cause severe pain and may also lead to bleeding during bowel movements. An anal fistula is a tunnel or tract that runs between the anal canal and the skin. It is associated with pus from the anal area. You can differentiate between the three conditions based on the symptoms you are experiencing. All of them can be prevented through lifestyle modifications such as eating a fibre-rich diet and increasing your fluid intake.




