Is your hospital or your doctor withholding your medical records? Read on to find out who can access these records.
Is it legal for hospitals to withhold medical records from patients or their authorised attendants?
What is the process for requesting medical records?
- To obtain medical records, you may be required to formally write a letter to the concerned authority in the hospital.
- The doctor or the hospital is legally bound to provide a copy of the said records to the patient or the authorised attendee within 72 hours of the receipt of the letter.
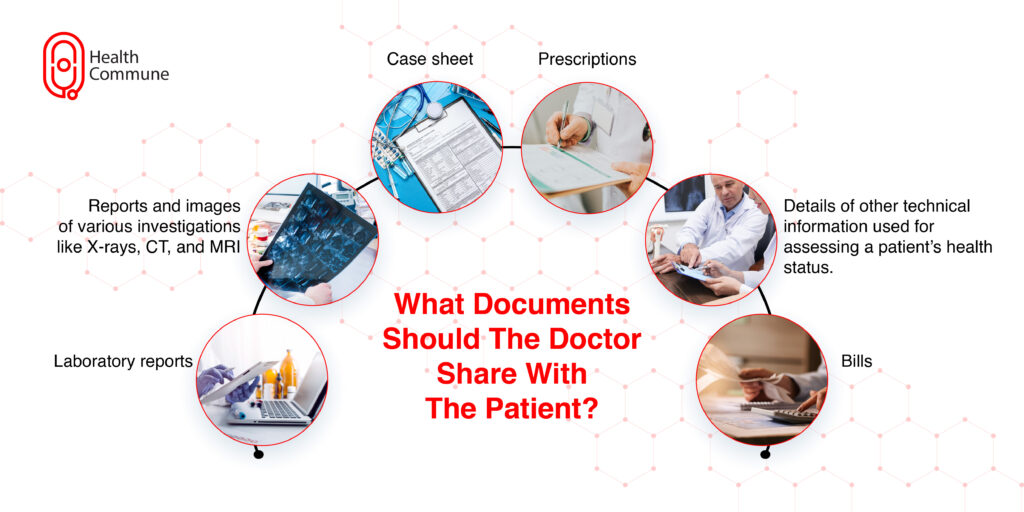
What are the different kinds of documents that the doctor should share with the patient?
- Case sheet
- Laboratory reports
- Reports and images of various investigations like X-rays, CT, and MRI
Bills - Prescriptions
- Details of other technical information used for assessing a patient’s health status.
Is it legal for hospitals to charge patients for copies of their records?
How long is the doctor or hospital obliged to store the medical records of a patient?
- The Medical Council of India (MCI) prescribes doctors to store the medical records of indoor patients for a period of up to three years.
- Not preserving the medical records for a three-year period is considered professional misconduct by the MCI
- However, there is no binding on the doctors to preserve the out-patient (OPD) records. Hence, patients should take all precautions to preserve their OPD records.
Is it necessary for the doctor to record every step of the treatment in the medical record?
Yes. The medical records should include the following details:
- Patient’s history
- Clinical findings
- Results of diagnostic tests
- Provisional diagnosis.
- Final diagnosis
- Pre-operative care (if applicable)
- Operation notes (if applicable)
- Post-operative care (if applicable)
- Daily notes on the patient’s progress and medications
- Consent forms
- Prescriptions (which should be legible and contain patient’s name, date, and the doctor’s signature)
- In case of the patient’s death, the cause of death certificate (MCCD)
Is there any previous court case in reference to this?
Case details: Mrs Anita Singh vs. Directorate of Health Services, GNCTD. Dated March 16, 2016. CIC/SA/A/2015/001894. Central Information Commission.
Background of the case:
Through a Right to Information (RTI) application, the patient’s mother sought the following information about her son’s treatment, who was admitted on 8.2.2015 and died on 3.3.2015 during treatment:
- Name of the consultant who treated the patient during the aforementioned time period
- Day-to-day treatment records
- Copy of the test report or test results conducted during the aforesaid period,
- The amount charged by the hospital during the period
The hospital replied: “Information is not available, and the hospital cannot disclose the documents, which are confidential to patients, to a third party in the absence of any authority letter from the patients or legal heirs.”
Central Information Commission order:
- The Commission, after perusing clause 1.3.2 of the Professional Conduct, Etiquette, and Ethics Regulation 2002, observed that patients and their relatives are entitled to know treatment details, including the names and qualifications and experience of doctors. As per the law, this information has to be given within 72 hours.
- The Commission also issued a show cause letter to the hospital, explaining why the mother of the patient should not be awarded compensation of Rs. 50,000.



